
In this post we have discussed the presenting chief complaints and the examination procedures of any disease related with Nervous System.
Here in this post , for your better understanding we have divided it into eight parts, and they are :
- What are the symptoms with the patient commonly present.
- Nervous system examinations.
- What are the physical examinations to be done.
- What are the examination of peripheral nerves
- What are the cranial nerve and their examinations
- What are the tests of the sensory system
- What are the examinations of the motor system
- And the investigations we do to check the nervous system diseases.
What are the symptoms with the patient commonly present
I. Headache :
This is the most common presenting feature. There can be two types of reason behind the headache that is Primary causes and Secondary causes.
- Primary causes – Primary stabbing and thunderclap headache, migraine(most common), headache due to anxiety and overthinking(this pain commonly held in occipital lobe), cluster headache, exertion headache by coughing, sex etc.
- Secondary headache – Mainly occurs due to subarachnoid haemorrhage and central vein thrombosis. Sometimes temporal arteritis also causes secondary headache.
II. Dizziness and vertigo :
- Dizziness – Lightheadedness, faintness, or the sensation that your head is spinning are all possible symptoms of an altered sense of balance and location. This can occur due to cardiac arrhythmia or hypoventilation which can occur due to anxiety or panic, other two causes are postural hypotension and cerebrovascular disease.
- Vertigo – An internal or outward spinning sensation brought on by moving your head too quickly. This mainly occurs due to problem in the vestibular apparatus and problems in the brain(less common).
III. Seizure :
A seizure is an uncontrollable electrical disruption in the brain that occurs suddenly. It can alter your behaviour, motions, or sensations, as well as your level of consciousness.
There are mainly three phase of seizure through which it occurs :
- Tonic Phase – This phase is characterised by the loss of consciousness, in addition with body stiffening.
- Clinical Phase – This phase is mainly characterised by the rhythmical jerking which lasts for approximately 30-120seconds.
- Postictal Phase – When the patient reorientates.
IV. Loss of consciousness for a short period of time :
SYNCOPE – This is known as loss of consciousness occurs due to poor cerebral perfusion. And this is known as the most common cause of transient loss of consciousness(TLOC).
Other causes of TLOC – 1. Cardiac cause, 2. Drugs like antihypertensive or levodopa, 3. Hypertension in diabetes.
V. Neurological symptoms with a functional component :
Sometimes patients can present with many neurological symptoms, which are not due to any disease.
Here the patient can present with various clinical features like :
- Blindness
- Weakness and collapsing attacks
- Tremor
- Pain and Lethargy
- Psychogenic and other mood disorders
- Anxiety
VI. Transient ischemic attack (TIA) and stroke :
TIA – A transient stroke-like event that, despite resolving in minutes to hours, need rapid medical intervention to differentiate from a true stroke.
Stroke – A transient stroke-like event that, despite resolving in minutes to hours, need rapid medical intervention to differentiate from a true stroke.
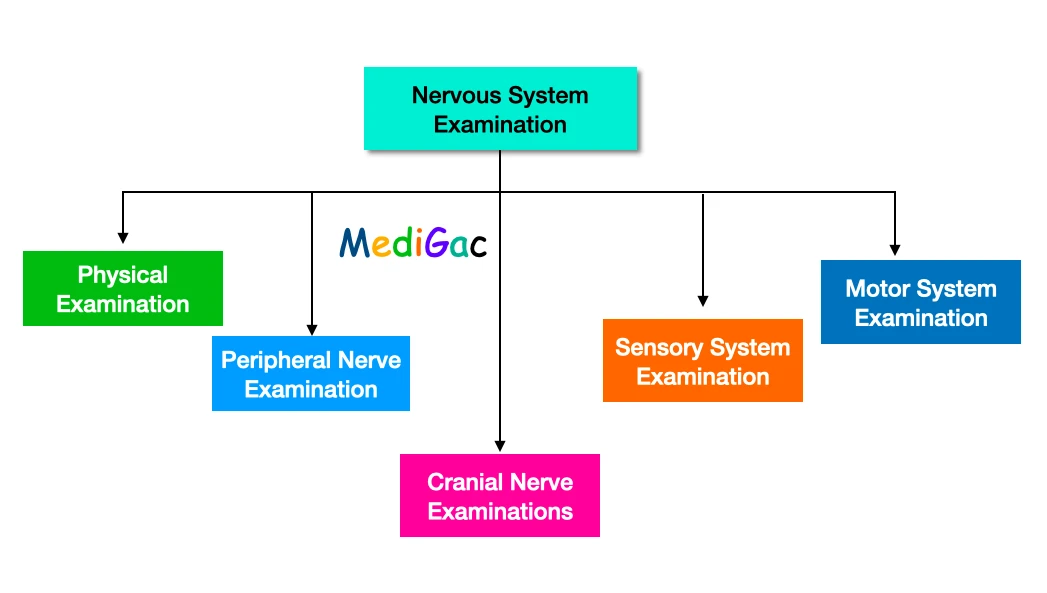
EXAMINATIONS DONE TO CHECK NERVOUS SYSTEM
So, in this chart we have seen that how many examinations normally we do for the examination of the nervous system. So here we have discussed five examinations ; Physical examination, Peripheral nerve examination, Cranial nerve examination, Sensory system examination and the motor system examination.
What are the Physical examinations to be done
I. Consciousness Checking :
To check the consciousness of a patient, we mainly use the Glasgow Coma Scale.
| Behaviour | Response |
| 1. Eye opening response | Spontaneously – 4 Response to speech – 3 Response to pian – 2 No response – 1 |
| 2. Verbal Response | Oriented to time, place and person – 5 Confused – 4 Inappropriate words – 3 Incomprehensible sounds – 2 No response -1 |
| 3. Best motor response | Obeys commands – 6 Moves to localised pain – 5 Flexion withdrawal from pain – 4 Abnormal flexion – 3 Abnormal extension – 2 No response – 1 |
II. Speech Testing :
Dysarthria is a motor speech condition that occurs when the muscles that create speech are injured, paralysed, or weakened. Dysarthria causes a person’s tongue and voice box to lose control, causing them to slur words. There are methods for improving communication.
Causes of Dysarthria :
- Upper and lower motor neuron lesions.
- Corticobulbar tracts lesions.
- Localised lesions of the tongue, lips or mouth.
- Pathology of the cerebellum and extrapyramidal system.
- Pathology of the nerve, muscle or neuromuscular junction.
III. Dysphasia :
A communication disorder in which a person’s capacity to communicate is impaired. There are two main area of the brain which causes the dysphasia. They are Broca’s area, Wernicke’s area.
- Damage to Broca’s area – This results in expressive dysphasia. And it shows reduced verbal output with non-fluent speech with the grammatical errors.
- Damage to Wernicke’s area – This can cause receptive dysphasia. In this case, the speech remains fluent but the comprehension gets deficient.
IV. Meningeal Irritation :
This is also known as meningism which is the inflammation of the meninges within the sub-arachnoid space. This can be detected by observing the resistance shown against the flexion of the leg.
Sometimes, non-neurological diseases can also cause meningeal irritation, they are Urinary tract infection and pneumonia.
Two signs are seen in meningeal irritation, and they are – Kernig’s sign and Brudzinsky’s sign.
- Kernig’s Sign – This sign is observed by seeing the resistance of the hamstring muscle against extension.
- Brudzinsky’s sign – When stiffness in the neck is present, then the neck can not be flexed possibly. And in response to neck flexion, the hips and knees gets flexed, this incidence is known as Brudzinsky’s sign.
V. Function of the cortex :
The cerebral cortex, which is the brain’s biggest section, is the brain’s ultimate control and information-processing centre. Many higher-order brain functions, such as sensation, perception, memory, association, cognition, and voluntary physical activity, are controlled by the cerebral cortex.
There are mainly four lobes which can divide the cortical functions – Frontal lobe, parietal lobe, temporal lobe and occipital lobe.
I. Frontal Lobe –
If any damage to the frontal lobe occurs, then some disorders can be seen there.
- Dysphasia
- Loss of emotional feelings
- Urinary incontinence
- Focal motor seizure
- Cognitive impairments (A person has trouble remembering, learning new things, concentrating, or making decisions that affect their everyday life.)
- Gaze of the eye
II. Parietal Lobe –
If any damage to the parietal lobe occurs, then some disorders can be seen there.
- Contralateral lower quadrantanopia
- Focal seizure
- Hamper of cortical sense
- Visuospatial disturbance
- Apraxia
III. Temporal Lobe –
If any damage to the temporal lobe occurs, then some disorders can be seen there.
- Dysphasia
- Focal seizure and also psychic symptoms
- Contralateral upper quadrantanopia
- Memory gets hampered
IV. Occipital Lobe –
Damage to this site can result in :
- Hemianopia or scotoma
- Hallucinations
- Visual agnosia
- Interruption of the visual perception
What are the examination of peripheral nerves

I. Radial Nerve :
A patient with radial nerve injury can present with mainly two abnormalities :
- Wrist Drop – Wrist drop is a medical disorder in which the wrist and fingers at the metacarpo phalangeal joints are unable to stretch. Due to the opposing activity of forearm flexor muscles, the wrist stays partially flexed. As a result, the posterior compartment’s extensor muscles remain paralysed.
- Saturday Night plays – Saturday night palsy is a radial nerve compression neuropathy caused by sustained, direct pressure from an object or surface on the upper medial arm or axilla. The C5 to T1 nerve roots, which come from the posterior section of the brachial nerve plexus, make up the radial nerve.
II. Ulnar Nerve :
Ulnar nerve palsy can occur due to the nerve damage, which can results in the weakness or loss of coordination of the fingers.
III. Median Nerve :
Damage to the median nerve can cause –
- Carpal tunnel Syndrome – Carpal tunnel syndrome, also known as median nerve compression, is a condition in which your hand feels numb, tingly, or weak. It occurs as a result of pressure on your median nerve, which spans the length of your arm, passes through the carpal tunnel in your wrist, and terminates in your hand.
IV. Lateral cutaneous nerve :
This nerve has a huge chance to get compressed under the inguinal ligament which can results in Paraesthesiae in the lateral thigh.
V. Common Peroneal nerve :
Damage to this nerve, commonly causes Foot drop.
- Foot Drop – Foot drop is a gait disorder in which the forefoot drops due to weakness, irritation, or damage to the common peroneal nerve, which includes the sciatic nerve, or paralysis of the muscles in the anterior lower leg. It is frequently a sign of a larger issue rather than an illness in and of itself.
What are the cranial nerves and their examinations

A. Olfactory(I) nerve examination :
Inquire if the patient has observed any changes in their sense of taste or smell. If this is the case, make sure the patient’s nostrils aren’t blocked and that he or she had not a cold recently.
Smell can be evaluated formally using smelling bottles where anosmia can be a precursor to Parkinson’s disease.
B. Optic(II) nerve examination :
Here we will check Visual acuity, Visual field, peripheral field, reflexes, ophthalmocospy and other eye tests.
A. Visual Acuity :
- To determine the best corrected visual acuity, ask the patient to wear glasses or contact lenses if necessary.
At a distance of 6 metres, visual acuity is measured using a typical Snellen chart. Request that the patient cover each eye in turn (you may need to do this for them) and read the smallest line of letters possible. - Informal testing include having the patient read a word on a piece of paper, such as your name tag, one eye at a time.
- Proceed in this order if the patient can’t read the largest letters on the Snellen chart or your badge with either eye:
Finger-counting
Hand motions
The ability to perceive light
The eye is said to have no perception of light if the patient sees nothing at all (NPL)
B. Visual Field :
- Confrontational testing of peripheral visual fields: the patient should look at your nose (and you at theirs). Ascertain that you and the patient are both sitting at the same horizontal level, 1 metre apart, with your glasses off.
- Ask the patient to stare at your nose and maintain their head motionless while you face them. Ask the patient to point to the finger that moves while holding your hands 60 cm apart. At the same time, wiggle both index fingers. When a patient is neglected, he or she will only notice one finger moving.
- PERIPHERAL FIELD –
For central scotoma, test each eye separately: can the patient see the entire face? To evaluate visual fields, put a white hat pin on each eye individually.
Otherwise, wiggle your finger:
- Start at the edge of your visual area and work your way towards the centre in well-defined increments). In each field, test the four quadrants.
- The red hat pin (which fades in optic neuritis) can be used to measure central visual fields, and the Amsler grid can be used to measure central vision.
- Goldmann kinetic perimetry and Humphrey visual fields tests can be used to formally measure visual fields.
C. Visual Reflexes :
- Size, shape, and symmetry of the pupils
- A direct reaction (brisk or sluggish, equal or unequal)
- Consensual reaction
- Accommodation reflex swinging light test for relative afferent pupillary deficit (RAPD) (pupil constricts on near-vision)
D. Ophthalmoscopy Tests :
- Red Reflex (15 degrees lateral to midline)
- Recognize the optic disc (colour, margins, central retinal vein pulsation)
- Ask the patient to look up and left, up and right, down and left, down and right to scan the retina (particularly the peripheries). To observe the retina on down gaze, you’ll need to lift their eyelid.
- Request that the patient stare directly at the light; this will ensure that you are looking at the macula.
E. Other Tests :
- Colour vision test – Ishihara Plates
- Blind spot – This is assessed with a red hat pin, when papilloedema occurs.
C. Trochlear(III), Trigeminal(IV) and Abducens(VI) nerve examination :
- Ask the patient to focus on the tip of a pen held 50cm in front of their nose.
- In the primary position, check for ptosis, nystagmus, and strabismus.
- Smooth pursuit : In the horizontal plane, move your finger quickly from left to right and back.
Look for nystagmus (pathological if >5 beats) at the extremes of your vision. - Hold one finger 50cm in front of the patient’s nose and a fist 50cm lateral to the finger for sporadic eye movements.
- In the lateral plane, ask the patient to transfer their sight quickly between fist and finger.
- Examine the speed and precision of these motions.
D. Trigeminal(V) nerve examination :
Tests of sensitivity :
Cotton wool can be used to assess the ocular (V1), maxillary (V2), and mandibular (V3) sensory branches.
Motor Inspect for masseter and temporalis wasting, then have the patient clench their teeth to evaluate power.
To assess pterygoid power, ask the patient to open his mouth and keep it open despite resistance (check for jaw deviation to the side of the lesion).
Reflexion :
Corneal reflex is a reflex of the cornea (afferent: V1, efferent VII)
Jerk of the jaw (afferent: V3, efferent: motor V)
E. Facial(VII) nerve examination :
Examine (facial asymmetry)
1. Raise the patient’s brows (forehead sparing in UMN lesion), scrunch up their eyes, blow out their cheeks, and reveal their teeth.
F. Vestibulocochlear(VIII) nerve examination :
In each of the patient’s ears, whisper a number. Request that they repeat it.
If hearing loss is discovered, provide the following tests:
- Rinne test (512Hz tuning fork)
- Weber’s test (512Hz tuning fork)
- audiometry are used to formally assess hearing loss,
- otoscopy
G. Glossopharyngeal(IX) and vagus(X) nerve examination :
Check for hoarseness and quietness in your speech quality and volume (dysarthria, dysphonia)
- Ask the patient to open their mouth and say ‘Ahhhh’ (examine for palatal asymmetry and uvular deviation away from the side of the lesion)
- Offer to test the left and right gag reflexes independently
- If the patient has any speech difficulties or aberrant palatal sensation/movement, refer them to SALT.
H. Spinal Accessory(XI) nerve examination :
- Request that the patient shrug their shoulders and hold them there despite resistance (trapezius)
- Request that the patient turn their head and push back against the examiner’s hand (sternocleidomastoid)
I. Hypoglossal(XII) nerve examination :
- Check tongue power against each cheek o Wasting and fasciculations in motor neuron illness
- Tongue deviation towards side of lesion in LMN pathology
- Tongue deviation towards side of lesion in LMN pathology
What are test of the Sensory System

I. Common Presenting Symptoms :
The sensory system mainly composed of simple sensations of light, temperature, pain, touch, and vibration.
Propioception(Joint position sensed) & higher cortical sensations which signifies two-point discrimination, stereognosis(in the absence of visual and aural input, the ability to comprehend and distinguish an object’s form), graphaesthesia(Guessing the numbers and letters drawn on th skin) and localisation.
Common problems of the sensory systems are described here. Patients can present with this kind of problems.
- Analgesia – This is the inability to feel the pain.
- Hyperalgesia – Hyperalgesia is a condition in which your pain sensitivity is increased. The increase in sensitivity of specific nerve receptors in your body causes this.
- Hypoaesthesia – This is the decreased sense of touch or sensation.
- Hyperaesthesia – A condition, where the patient feels excessive physical sensitivity especially through the skin.
- Paraesthesia – Pressure on or injury to peripheral nerves causes an odd feeling, usually tingling or pricking.
- Allodynia – Allodynia is a situation in which a stimulus that does not typically trigger pain causes pain.
Examination Sequence –
- Light touch feeling – Done by using a cotton wool to wisp.
- Superficial skin sensation – Using a fresh neurological pin.
- Checking the temperature – Using a cold metallic object.
- Vibration feeling – Using the Tunic fork.
- Proprioception
- Stereognosis and graphaesthesia – Using a familiar object like a coin.
- Sensory inattention – Touching of limbs and asking them which side of it is.
II. Sensory Modalities :
This is the finding of the cause of the lesion, and where the lesion is affecting. Like it is in the peripheral nerves, dorsal roots or spinal cord or intracranial.
A. Peripheral nerve and dorsal root –
- Lower Limbs – Normally peripheral neuropathy tries to affect the lower limbs which first seen on the toes.
- Upper Limbs – Neuropathy in the upper limb suggest a disease located in the spinal cord and demyelinating rather than axonal neuropathy.
Rather than the somatic neuropathy, autonomic system also can get affected. This can result in sweating, sphincter control and the cardiovascular system.
B. Spinal Cord –
Injury to spinal cord can result in some sensory disorders.
- Syringomyelia – The term “syringomyelia” refers to a condition in which a cyst or cavity forms within the spinal cord.
- Hyperaesthesia – A condition, where the patient feels excessive physical sensitivity especially through the skin.
C. Intracranial lesions –
Normally suggests brain stem lesions.
- Lower brain stem lesions – This might result in ipsilateral facial numbness as well as contralateral body numbness.
- Thalamic lesions – This can result in patchy sensory impairment on the opposite side, as well as unpleasant, poorly localised pain that feels like it’s burning.
Examination of the Motor System

I. Checking the Tone of the muscle :
The tension in a muscle at rest is referred to as muscular TONE. It is the muscle’s reaction to an external force, such as a stretch or a direction shift. Our body can swiftly respond to a stretch if we have the right muscle tone.
There can be two types of muscle tone :
- Hypotonia – Lower motor neuron lesions can cause decreased tone, which is frequently accompanied by muscular atrophy, weakness, and hyporeflexia.
- Hypertonia – Due to spasticity and rigidity, muscle tone increases.
- Myotonia – Myotonia is a series of neuromuscular illnesses characterised by the inability of muscles to relax correctly, the most prevalent of which is myotonic dystrophy.
- Clonus – Clonus is a rhythmic series of contractions triggered by a rapid muscle and tendon strain and this can be due to upper motor neuron lesion.
II. Inspection and Palpation of the Muscles :
Here we check for the muscle mass, fasciculation and Abdominal movements
A. Muscle Mass –
Mainly lower motor neuron disorders can cause loss of muscle mass whereas no effect in upper motor neuron disorders.
B. Fasciculation –
When individual motor unit fires spontaneously, then the muscles shows visible irregular twitching. These are known as fasciculation.
C. Abdominal Movements –
- Myoclonic Jerks – These are single or recurrent, abrupt, shock-like contractions of one or more muscles that can be localised or diffuse.
- Tremor -Tremor is an involuntary oscillatory movement around a joint or a group of joints caused by muscular contraction and relaxation. Can be caused by Hyperthyroidism, excess alcohol intake, abnormal neck postures like torticollis, antecollis, retrocollis.
III. Checking the deep tendon reflex of muscles :
When a muscle response against a stretch, a involuntary contraction is produced this is known as a tendon reflex.
Other reflex tests we commonly do :
- Hoffmann’s reflex
- Abdominal reflexes
- Finger jerk
- Cremasteric reflex – only present in males
- Plantar response
IV. Primitive reflex checking :
In reaction to certain stimuli, primitive reflexes are reflex acts originating in the central nervous system that are displayed by normal babies but not neurologically intact adults.
V. Stance and Gait examinations :
Intact ocular, vestibular, sensory, corticospinal, extrapyramidal, and cerebellar pathways, as well as functioning lower motor neurones and spinal reflexes, are source for stance and gait.
Causes :
- Cerebrovascular disease
- Hydrocephalus
- Cerebellar disease
- Spinal cord lesions
- Parkinson’s disease
- Macular dystrophies
- Neuropathies
- Common perineal nerve palsy
VI. Coordination testing :
Coordination is defined as a healthy sensory and motor system, as well as a healthy cerebellum, to perform complicated movements smoothly and efficiently.
Different tests we do to check coordination :
- Finger-to-nose test
- Heel-to-shin test
- Rapid alternating movements
VII. Checking the power of the muscle :
Using MCR(Medical Research Council) Scale we can detect the strength of muscle.
| Grade | Description |
| 0 | No muscle contraction visible |
| 1 | Flicker of contraction but no movement |
| 2 | Joint movement when effect of gravity eliminated |
| 3 | Movement against gravity but not against resistance |
| 4 | Movement against resistance but weaker than normal |
| 5 | Normal power |
Upper motor neuron lesions – This mainly produce weakness of large group muscles.
Lower motor neuron lesion – This can cause weakness of specific or individual muscle.
The investigations we can do to check nervous system
- DaTscan – DaTscan is a technology used to confirm a Parkinson’s disease diagnosis. It’s a form of SPECT imaging technology that helps visualise dopamine transporter levels in the brain.
- CT Scan – Computed tomography scan
- Unenhanced computer tomogram
- MRI – Magnetic Resonance imaging
- HRCT – High resolution CT
- CECT – Contrast enhanced CT
Specific Investigations :
- Lumbar Puncture – CSF sample is taken and are routinely examined to see the cell count, protein content, and glucose level. In different types of meningitis, we also take the CSF sample.
- Neurophysiological tests – EEG(Electroencephalography) helps to record the spontaneous electrical activity inside the brain.