We have discussed all the examinations of breast in this article. The list of discussion is mentioned below.
- General examination
- Systemic/local examination
- Surrounding structures examinations
- Lymph nodes examination
- Special investigation procedures
1. What are the general examination
- In the case of gynecomastia, a thorough medical history should be taken initially.
- Liver examination – The liver should be checked for secondary deposits in cases of breast cancer, Cirrhosis should also be checked.
- Lungs and bones examination – Lungs and bones, especially the ribs, spine, sternum, pelvis, higher ends of the femur, and humerus, should all be checked for metastases.
- Rectal and vaginal examination – Krukenberg’s tumour of the ovary, which is caused by transcoelomic implantation or lymphatic penetration.
- Anorchism, cryptochism, teratoma, and chorionepithelioma should all be checked.
- Males with associated leprosy may have breast hypertrophy.
- During puberty, certain drugs, like as breast augmentation in males, are seen, which is deemed typical.
2. What are the examinations of breast :

During the examination of breast, we mainly follow the rule of Inspection and palpation. Here we don’t apply the percussion and auscultation methods.
I. What are the Inspection methods :
In inspection we mainly follow up four principles –
- The arms will be placed by the side of the body.
- When she raises her arms straight above her head, the bump or dimple may be more noticeable.
- When aberrant movement of the nipple or exaggeration of skin dimples is seen, place her hands on her hips and press and relax as the physician instructs.
- Bending forward from the waist, allowing the breasts to slip away from the torso. Any nipple that does not slip out from the chest is a sign of abnormal fibrosis behind it. The entire breast should be inspected in a systematic manner.
1. Examination of breast tissue/mass :
We look for puckering or dimpling, as well as the position, size, and shape.
- Position – whether or not it has been shifted in any direction.
- Dimensions and shape – whether it is larger or smaller than its companion. Gynaecomastia is a condition in which a man’s breasts expand.
- Any puckering or dimpling – In scirrhous carcinoma, the breast may shrink and draw inwards towards the tumour. Lifting the breast slightly upwards might bring out dimpling in the skin.
2. Examination of nipple of breast :
During the inspection of nipple, we mainly check for presence, position, number, size and shape, surface, eczema, if any discharge is present.
- Presence – First, we’ll look for the presence of a symmetrical breast nipple or one that has been retracted or destroyed.
- Position – The position of both sides’ nipples should be carefully compared.
- Number – In addition to the conventional nipples, accessory nipples may be present. The milk line, which runs from the axilla to the groin, is where they are most commonly observed.
- Size and shape – It should be evaluated for size and shape to see if it is prominent, flattened, or retracted.
- Surface – During the inspection of the surface of the breast, we must check for the fissure, cracks and eczema.
- Discharge – The kind of the discharge is examined, as well as whether it originates from the direct nipple or the surrounding area.
3. Examination of skin over the breast tissue/mass :
During inspection of the skin over breast we mainly check for colour, texture, engorged veins, dimple, retraction or puckering, and Peau d’orange appearance.
- Colour and texture – The skin becomes red, heated, and oedematous in acute mastitis. A similar appearance might be seen in acute mastitis carcinomatosa on rare occasions.
- Engorged veins – Engorged veins are seen frequently in big soft fibroadenomas and quickly developing sarcomas.
- Dimple, retraction – This is frequently observed in breast scirrhous cancer.
- Peau d’orange – It’s a term for a condition in which the skin gets thick and pitted, with a texture and appearance similar to orange peel. Skin redness and soreness, scaling, and a dark tint are all possible symptoms.
- Nodules – This can be seen in breast cancer, which is frequently metastatic.
- Ulceration and fungation – Ulcers can appear on any region of the skin. Fungus of the skin, on the other hand, is a late symptom of advanced breast cancer caused by the development of the skin.
4. Examination of areola of breast tissue/mass :
During the examination of the areola, we mainly focus on colour, size, surface and texture.
During the inspection it is seen that normal areola shows corrugated and contains Montgomery’s glands, which are tiny nodules. Montgomery’s tubercles are the result of these glands becoming larger during pregnancy.
- Colour – The skin of a young girl’s areola is pale pink, but it darkens significantly as she grows older and turns brown during pregnancy.
- Size – When a soft fibroadenoma or sarcoma causes a significant swelling, the size of the areola increases.
- Surface and texture – During the inspection we mainly check for cracks, fissures, ulcers, eczema, edoema, and discharge, among other things. The areola develops bright red in the early stages of Paget’s disease and is eventually eliminated, leaving a red weeping ulcer.
II. What are the Palpation methods :
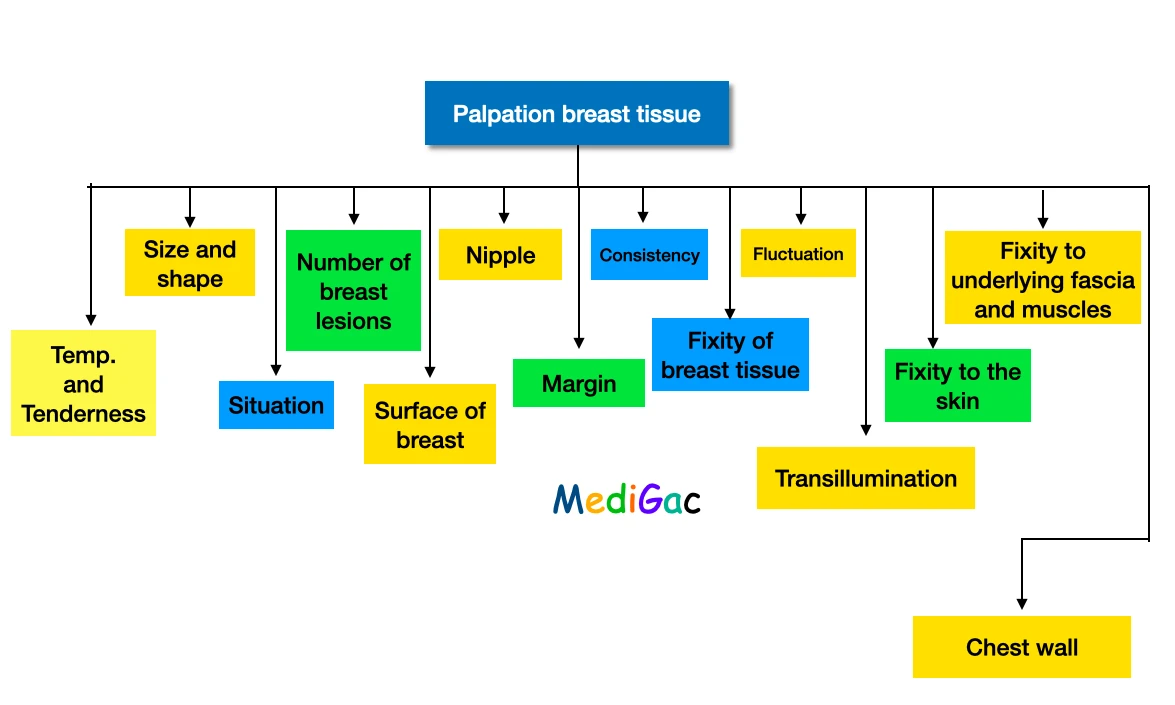
- Palpation should begin in a sitting position, then progress to a semi-recumbent 45-degree position, and finally to a recumbent position.
- It’s best to start by palpating the normal breast.
- Palpation should be done with the palmar surface of the fingers while holding the hand flat, not with the ‘flat of the hand,’ as this implies using the palm of the hand, which is incorrect.
- The affected side is now palpated in the same way as the normal side, with the findings of the normal side compared to those of the affected side.
- Palpate the four quadrants in a systematic manner.
- You should also feel the axillary tail.
1. Examination of local temperature and tenderness :
- We mainly use back of the fingers which are the ideal place to feel/record the local temperature.
- When a warm and sensitive swelling is formed, which is usually the result of inflammation.
- However acute mastitis carcinomatosa which is know as inflammatory carcinoma, can also appear with identical symptoms.
2. Examination of size and shape of breast :
- A smooth surface is a sign of a healthy condition, whereas an uneven/irregular surface is a sign of cancer.
3. Examination of situation of breast :
- Normally carcinoma of the breast can develop anywhere in the breast, including the axillary tail but it is seen that occurrence of carcinoma is most frequent/common in the upper and outer quadrants.
- Fibroadenoma(Non-cancerous) is more common in the bottom half of the breast than in the upper half, but it can appear anywhere in the breast.
- Fibroadenosis(Non cancerous benign growth) is more common in the upper and lower quadrants, as well as the axillary tail.
4. Examination of number of breast :
- There is a fact that the majority of breast lesions are single, Fibroadenosis is recognised for its multiplicity.
- If there are several lumps to be felt then this can be possible that the opposite breast is also affected as well.
5. Examination of surface of breast :
- Benign tumour is globularly encapsulated and has smooth surface.
- Whereas carcinoma has a stony hard consistency. In the case of sarcoma, consistency may differ from one location to another.
6. Palpation of the nipple :
- It’s critical to palpate the nipple as well as the breast tissue directly below the nipple.
- Tumors that are located close to the nipple are frequently adhered to the nipple.
- To assess if the underlying lump causes or promotes nipple retraction, the underlying lump is relocated.
- Gentle pressure on such a tumour may cause nipple discharge.
- Take note of its visibility and try to figure out whether it’s blood, serum, pus, or milk. After that, a bacteriological culture should be performed on the material.
7. Examination of margin of breast :
- The borders of fibroadenosis are ill-defined.
- The margin of a fibroadenoma is regular and tends to slip away from the palpating fingers.
- But the margin of a carcinoma is highly irregular and does not tend to slip away from the palpating fingers because it is fixed to the breast tissue.
8. Examination of consistency of breast :
- The examiner should check the consistency of the lump, whether it is cystic, firm, hard, or stone hard, must be appropriately analysed.
- Then we must have to check for any fluctuation if the patient has a soft cystic swelling.
- Fibroadenoma is a hard tumour that develops in the axillary region.
- Fibroadenosis is characterised by a strong, widespread rubbery sensation.
9. Testing the fixity to the breast tissue :
- This is performed by gently manipulating the tumour with one hand while grasping the breast tissue with the other.
- A fibroadenoma is a benign tumour that is not attached to the breast tissue and can move around freely within the breast material.
- A carcinoma, on the other hand, is permanently attached to the breast tissue and cannot be moved.
- Fibrous filaments can be felt radiating into the breast material from the lump.
10. Examination of fluctuation of breast :
- The examiner should check the fluctuation of a cystic swelling.
- The clinician takes a position in front of the patient, who is seated on a table.
- Examiner’s two hands should be above the shoulder of the sufferer.
- Then the examiner holds the cyst in one hand and gently taps the cyst’s centre with the index finger of the other hand.
- The fluctuation test will be positive in chronic abscess and lipoma, in addition to cysts.
11. Performing transillumination test :
- This can only be done effectively in a dark room.
- The torch is held on the underside of the breast, directing the light through the breast tissue to the examiner.
- A solid tumour is opaque, whereas fat is translucent.
12. Testing of fixity to the skin :
This test can be done in three different ways:
- Attempting to move the tumour side to side or up and down will result in the skin dimpling or tethering.
13. Testing of fixity to the underlying fascia and muscles :
- The lump is first pushed in the direction of the pectoralis major fibres, then at right angles to them for as long as possible. The lump can be moved in both directions.
- The patient is now instructed to tighten her hip.
- Compare the range of mobility by moving the lump again in the same directions.
- Any mobility restriction along the line of the muscle fibres if it is fixed to it, although minor movement along the right angle of the fibres may be permitted.
14.Testing of fixity to the chest wall :
It is fastened to the chest wall if the tumour is fixed regardless of muscular contraction.
3. What are the examinations of surrounding structures of breast :
1. Examination of arm and thorax of breast tissue/mass :
- After completing the breast examination, a short examination of the affected side’s arm and the thoracic wall may provide useful information.
- The arm and chest wall may have several malignant nodules and thickened infiltrating skin that looks like a coat of armour.
- Extensive neoplastic involvement of the axillary lymph nodes may cause brawny oedema of the arm.
- Lymphatic obstruction is the main cause. After a radical mastectomy, an oedematous arm may appear.
2. Examination of axilla and supraclavicular fossa :
These areas should be thoroughly examined for any edoema caused by swollen lymph nodes. The pupils should make it a practise to inspect these areas so that they are never overlooked. The learner must also palate these regions in addition to the region.
3. Raising patient’s arms above her head :
This is the final step in the inspection process and should not be overlooked. Lifting the arms causes a shift in the contour of the breast that often displays lumps, puckering, and distortion that are not evident when the arms are by the sides.
4. What are the lymph nodes examination :
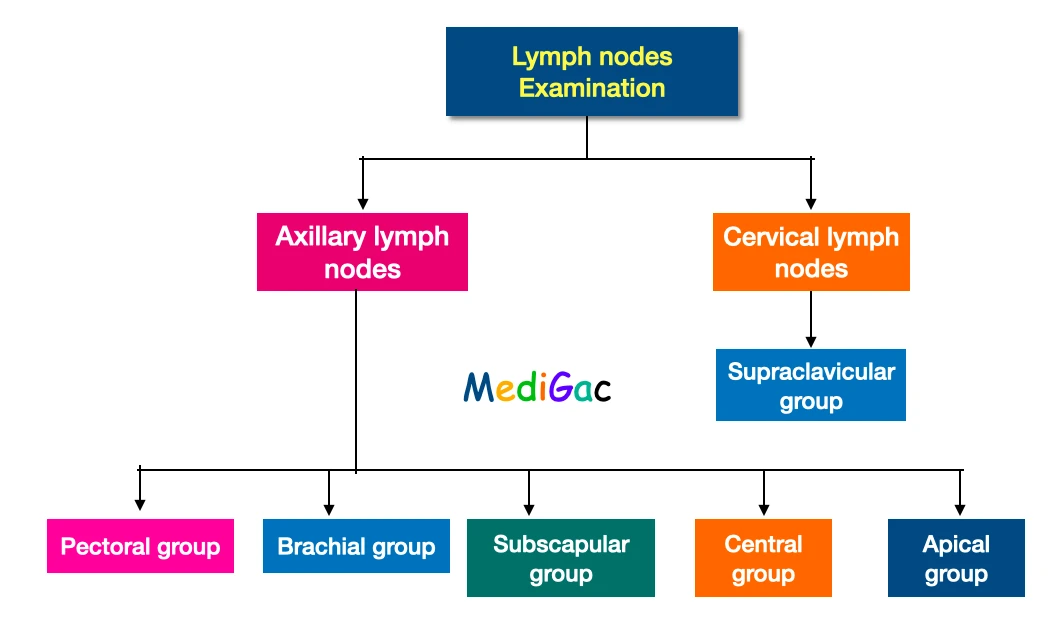
A. How to palpate the axillary group of lymph nodes :
In axillary group of lymph nodes palpation, we palpate mainly the Pectoral, Brachial, Subscapular, Central, and Apical group of lymph nodes.
I. Palpation of Pectoral group of lymph nodes :
- Just behind the anterior axillary fold lies this group.
- During the examination the patient is asked to raise his arms, and the fingers of the right hand are positioned behind the pectoralis major on the left side.
- The arm is then lowered down as well as should be resting on the forearm of the examiner.
- The pectoralis minor will show relaxation as a result of this.
- Then the examiner tries to palpate the lymph nodes with the pulps of the fingertips.
- The pectoralis major is pushed backwards from the front with the thumb of the same hand.
II. Palpation of Brachial group of lymph nodes :
- This group of lymph nodes is found on the lateral wall of axillary vein.
- The palm of the left hand is directed laterally against the upper end of the humerus to palpate this group.
III. Palpation of Subscapular group of lymph nodes :
- This is best inspected from behind and is located on the posterior axillary fold.
- The examiner stands behind the patient and palpates the antero-internal surface of the posterior fold with one hand while the patient’s arm is semi-flexed with the other.
- The nodes are now palpated while resting on this surface and looking backwards with the palm of the examining hand.
IV. Palpation of Central group of lymph nodes :
- With the right hand, we have to study this group on the left side.
- The patient is asked to abduct his/her arm laterally, with the extended fingers passing straight up to the axilla’s apex, directing the palm towards the lateral thoracic wall.
- The patient’s arm has been moved to the side of her body, and her forearm is now resting comfortably on the clinician’s forearm.
- To keep the patient steady, the clinician’s other hand is now placed on the opposite shoulder.
- Palpation is done by sliding the fingertips on the chest wall until the lymph nodes slip out from between the fingers.
V. Palpation of Apical group of lymph nodes :
- The examination is conducted in the same fashion as the last one, except that the fingers are pushed higher.
- If the lymph nodes are large enough, they can push through the cavipectoral fascia and be felt through the pectoralis major immediately below the clavicle.
B. How to palpate the cervical lymph nodes :

We mainly focus on the Supraclavicular group of lymph nodes. Lymph nodes above the collarbone that can be felt in the supraclavicular fossa are known as supraclavicular lymph nodes.
5. What are the investigations methods :
- Aspiration is done incase of any cystic lump is found.
- Biochemical studies – Liver metastasis is measured by elevated alkaline phosphatase and gamma glutamyl transaminase.
- Biopsy – Needle biopsy is an alternative excision procedure. The biopsy sample is further checked for any kind of malignancy.
- Bone Scan – As the name implies, it is specially made for bony metastases.
- Liver Scan – Metastases inside the liver is diagnosed.
- Chest X-Ray – This radiography test is mainly done to check any visceral metastasis.
- Bone X-Ray – This is a type of X-Ray which is usually done for pelvis, spine and upper ends of humerus and femur.
- Computerised tomography/CT Scan – This is usually done to detect mediastinal or retroperitoneal masses of malignant lymph nodes.
- Ultrasound – To find any cystic swelling
- Mammography is done to confirm any malignancy or carcinoma.
- Thermography – This is also done to check any malignancy of breast.