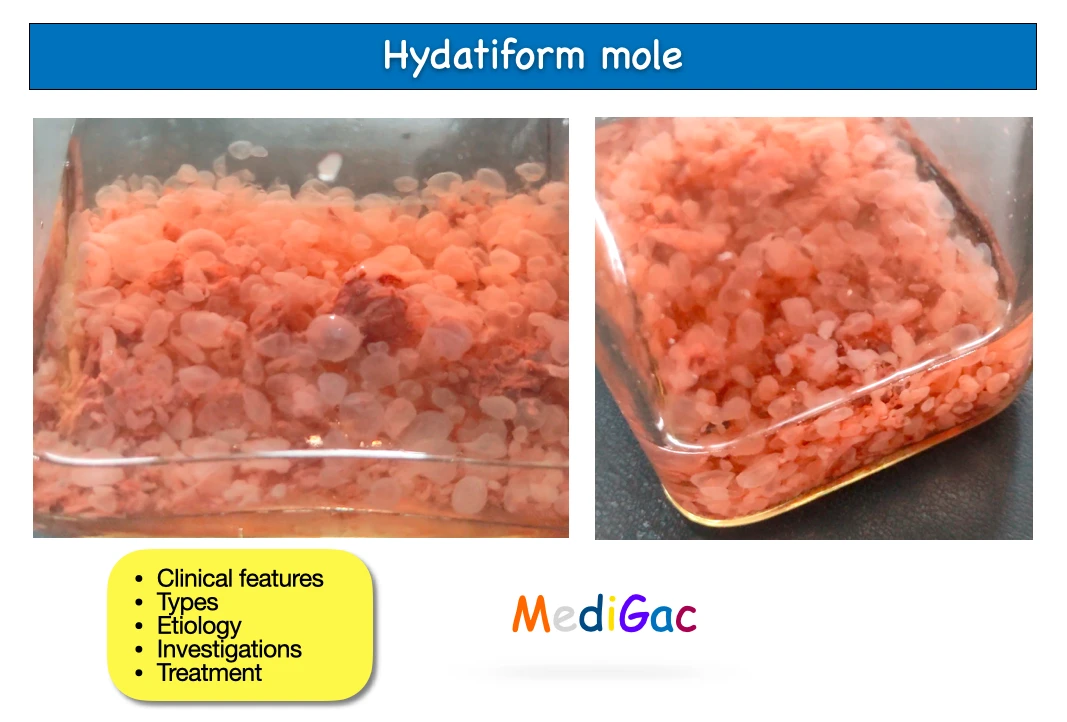
It is an aberrant placental syndrome where the immature chorionic vili undergo partially proliferative and partially degenerative alterations. These lead to the development of variously sized clusters of tiny cysts. Hydatidiform mole is the name given to it because of its outward resemblance to a hydatid cyst.
1. Clinical features :
- Vaginal bleeding with gelatinous mixed fluid.
- Lower abdominal pain.
- Vomiting in pregnancy.
- Breathlessness.
- Absence of FHS.
- Features of Hyperthyroidism (Tremors/tachycardia).
- Sick facial expression.
- Presence of pallor.
- Features of pre-eclampsia a like edema, hypertension.
2. Types :
| Complete Mole | Partial Mole |
| 1. Most common type seen. 2. No foetal parts found. 3. Chromosomal Diploid in nature. 4. Karyotype is 46XX(90%) & 46XY(10%). | 1. Identifiable foetal parts can be found. 2. Chromosomal Triploid in nature. 3. Karytotype is 69,XXX or 69.XXY. |
3. Pathophysiology/Etiology :
We are discussing the pathophysiology according to the types of moles. That is Partial mole and complete mole.
A. Partial Mole Formation/Etiology/Pathophysiology :
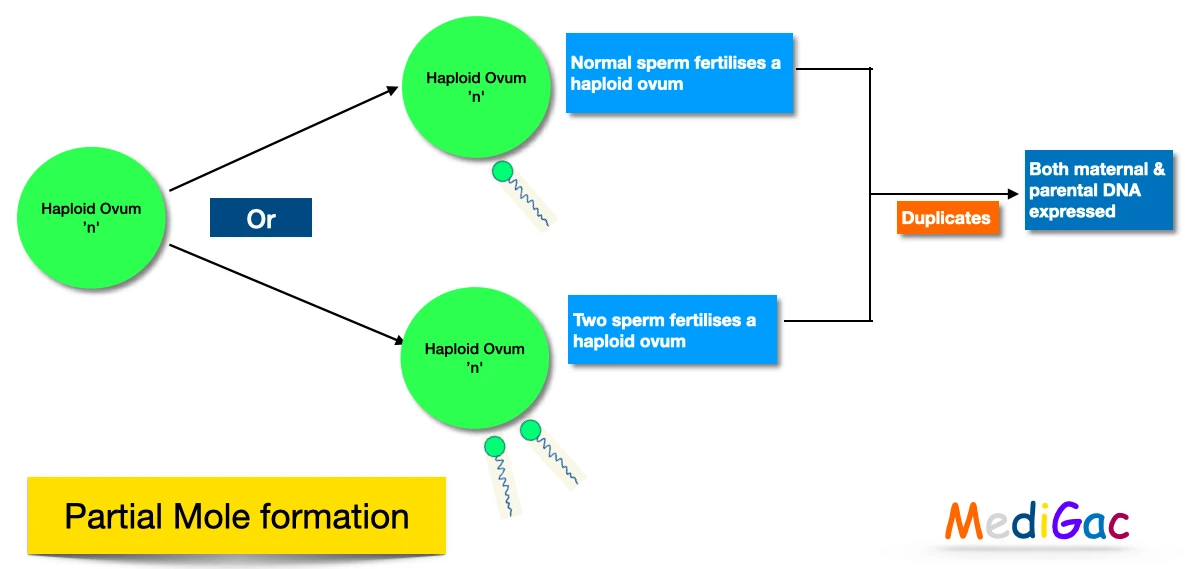
- Haploid ovum makes fertilisation with normal sperm or Two sperms fertilises a haploid ovum. Then it duplicates and both maternal & paternal DNA expressed.
B. Complete Mole Formation/Etiology/Pathophysiology :
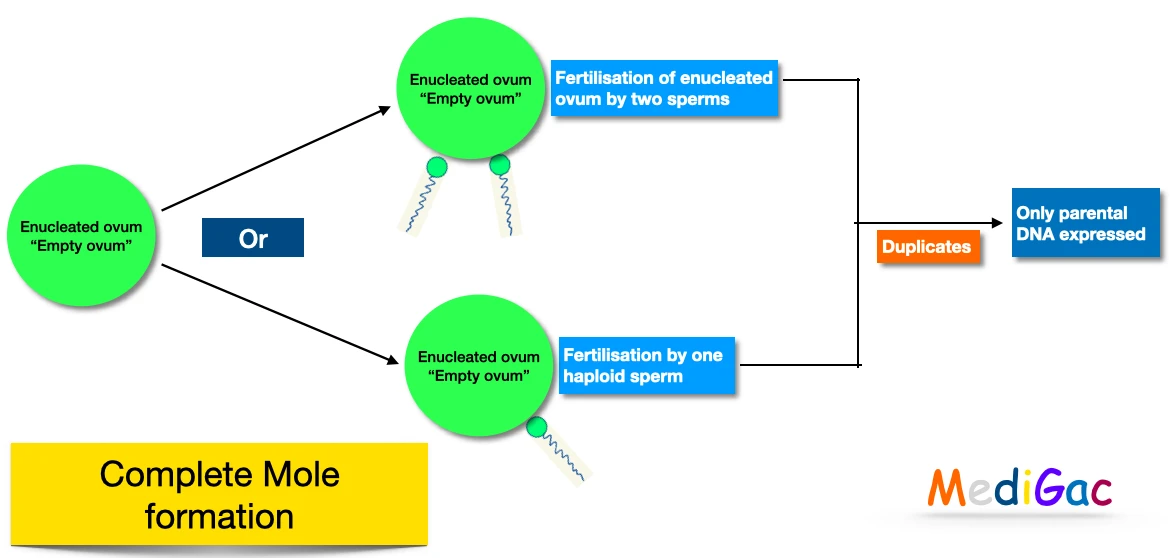
- Enucleated ovum or “Empty ovum” , Fertilisation done by two sperms or one haploid sperm. Further duplicates and forms products where only parental DNA expressed.
4. Investigations :
- Full blood count.
- ABO & Rh grouping.
- USG abdomen – ‘Snowstorm appearance’ is seen.
- Plain X-Ray Abdomen – Absence of foetal shadow and uterus size more than 16 weeks.
- CT and MRI – Usually not recommended if USG, Xray able to find out.
- Histopathological examinations of the out products confirms the diagnosis.
5. Treatment :
- Suction and evacuation of the uterus.
- Supportive therapy like treatment of anaemia and infection.
- Follow up counselling.