All the paediatrics/newborns/neonates nervous system examination. Higher psychic/cerebral function, Cranial nerves, motor-sensory, coordination, gait-posture, skull-spine, and primitive reflex We have discussed the paediatrics nervous system clinical examinations in 10 main topics, and they are :
- What are the common presenting symptoms
- What are the higher psychic or cerebral functions
- What are the primitive reflexes
- What are the Neurological Reflexes
- What are the cranial nerve examinations
- What are the sensory system examinations
- What are the motor system examinations
- How to check gait and posture
- What are the signs of meningeal irritation
- How to examiner skull and spine
- How to check coordination
I. What are the common presenting symptoms :
We have discussed all the common presenting symptoms or clinical features of most common nervous system diseases or disorders.
II. What are the higher psychic or cerebral function :
These includes
- knowledge
- Guidance
- Memory
- Focus
- Judgement
- Dyspraxia
- Dysarthritic disease
- Dysphonia
- Thinking
- Expression of the facial.
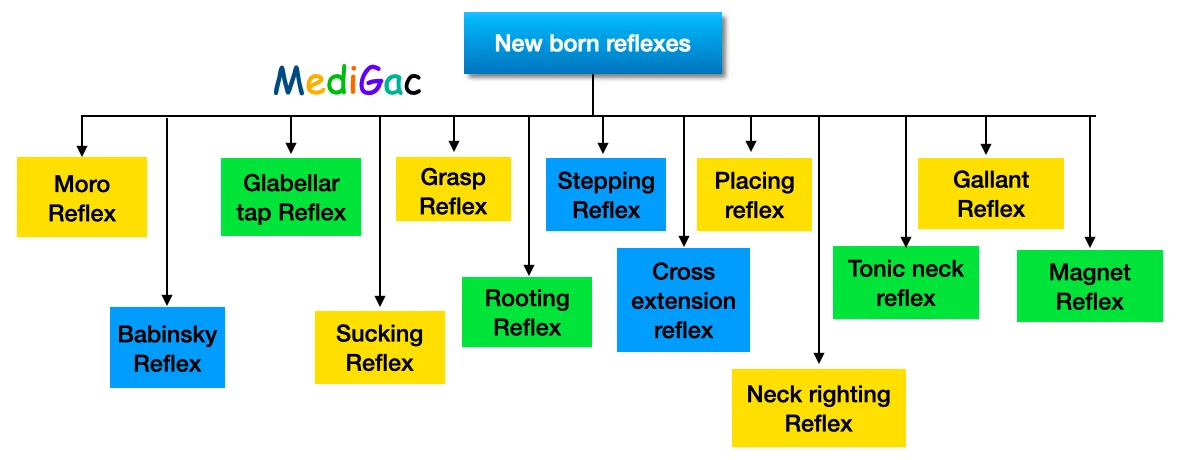
III. What are the newborn reflexes :
There are almost 13 types of reflexes are seen in a newborn, and they are mentioned below.
To read all the newborn reflexes in details please click on the below button.
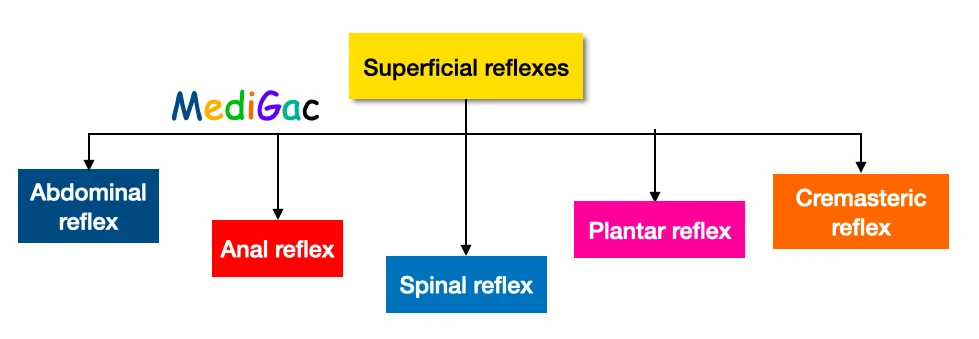
IV. What are the neurological reflexes
There are mainly two types of reflexes are seen, and they are – Superficial and Deep tendon reflexes.

To read all the superficial and deep tendon reflexes in details, please click the below button.
V. What are the cranial nerves examinations :

To read all the cranial nerve examinations in details, please click on the given below button
VI. What are the Sensory system examinations :
We mainly check three modalities of sensations, and they are – Crude sensations, Fine sensations, and Cortical sensations.
1. Crude sensations :
- Crude touch is a test that involves touching the skin.
- A fresh pin is used to test pain.
- Temperature is measured using metal tubes filled with cold (5-10 degrees Celsius) and heated (40-45 degrees Celsius) water.
2. Fine sensations :
- The exquisite touch sensation is evaluated using a wisp cotton wisp.
- The sense of vibration is examined.
- The feeling of the muscles is examined.
- The sense of proprioception, or sense of location, is also examined.
3. Cortical sensations :
We look for :
- localization by touch
- Inattention to the senses
- Discrimination on two levels
- Graphaesthesia
- Weight discrimination based on stereotypes
VII. What are the Motor system examinations :

In Motor system examination, we check for mainly four things – Bulk of muscle, Tone of muscle, Power or strength of muscle, and Reflexes
1. Bulk of muscle :
The examiner searches for any wasting, hypertrophy, or pseudohypertrophy throughout this evaluation (duchene).
Muscle wasting can be caused by a variety of factors, including :
- Myopathy is a condition that affects people.
- Malnutrition due to a lack of protein and calories
- Muscle atrophy due to inactivity
- Peripheral neuropathy (PN)
2. Tone of muscle :
The tension in a muscle at rest is referred to as muscular TONE. It is the muscle’s reaction to an external force, such as a stretch or a direction shift. Our bodies can quickly respond to a stretch when they have the right muscle tone. Tone of muscle is the resistance felt by the examiner while moving a joint passively.
Hypotonia :
This is Lower motor neuron illness causes hypotonia, which is characterised by muscular loss, atrophy, and hyporeflexia. Hypotonia is of two types Spasticity and Rigidity.
Spasticity –
- Spasticity is a characteristic of upper motor neurone injury that is velocity dependent and resistant to passive movement.
- Weakness, hyperreflexia, an extensor plantar response, and sometimes clonus are all common symptoms.
- This is detached as ‘catch’ at the start or conclusion of passive movement in a modest form.
- This can restrict range of motion and be linked to contracture in extreme cases.
- This is more noticeable in the upper limb when attempting extension, and in the legs when attempting flexion, such as walking.
Rigidity –
- Rigidity is a type of resistance that persists over a range of motion and can be detected when a limb is moved slowly.
- This is known as ‘lead pipe rigidity’ in parkinsonism.
- In the presence of parkinsonian tremor, the movement may be interrupted on a regular basis, giving it a jerk or cog wheeling effect.
Clonus :
- Clonus is a rhythmic series of contractions triggered by a rapid muscle or tendon strain. Clonus that is not sustained and lasts less than 6 beats could be physiological.
- Sustained clonus, on the other hand, indicates upper motor neuron injury and is frequently accompanied by spasticity.
Paratonia(Gagenhalten) :
When the examiner tries to move the patient’s limb, he puts up vigorous resistance, which is typical of a demented patient in a stupor.
3. Power or strength of muscle :
This is normally done by resisting the patient’s muscle activity. Individual muscle groups, such as the flexion/extension group in the upper and lower limbs, the trunk, and the neck, can be examined.
For instance, the abdominal muscle can be examined by asking the patient to sit up from a flat position with his or her arms folded over his or her chest.
4. Reflexes :
We have discussed earlier in this post, but still we are providing the link where these things are discussed in details :
VIII. How to check Gait and posture :
During locomotion, a gait is a pattern of limb motions. The numerous ways in which a human can move, either naturally or as a result of specific training, are referred to as human gaits.
Types of gait :
There are mainly eight types of gait which are classified according to their causes, i) Neuromuscular causes, ii) Other causes
I) Neuromuscular causes :
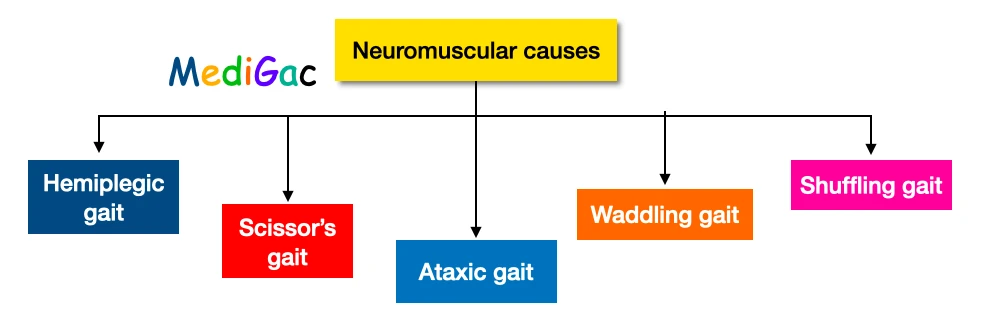
According to the neuromuscular causes, there are mainly five types of gait, and they are Hemiplegic gait, Scissor’s gait, Ataxic gait, Waddling gait, Shuffling gait.
- Hemiplegic gait – Hemiplegic gait is characterised by a loss of normal hip and knee swing, as well as leg circumduction. To provide appropriate circumduction on the affected side, the pelvis is frequently rotated upward. The leg travels forward and then swings back toward the midline in a circular motion during ambulation. e.g., Congenital cerebral palsy or acute stroke syndrome can cause spastic hemiparesis.
- Scissor’s gait – Scissor gait is a type of gait anomaly most commonly seen in people with spastic cerebral palsy. An upper motor neuron lesion is linked to that disorder and others like it. e.g., spastic paraplegic cerebral palsy, spastic diplegia cerebral palsy.
- Ataxic gait – Ataxic gait is characterised by an uneven foot placement, a wide base, and instability due to a lack of muscular synchronisation. e.g., peripheral sensory loss, cerebellar ataxia due to cerebellar diseases.
- Waddling gait – Waddling gait, often called myopathic gait, is a walking style. Muscle weakness in the pelvic girdle, a bowl-shaped network of muscles and bones that connects your torso to your hips and legs, causes this condition. e.g., Duchenne or Becker myopathy
- Shuffling gait – A shuffling gait is a walking style in which a person drags his or her feet. The term “shuffle gait” refers to a walking style in which the foot is still moving when it lands. e.g., spasticity of both lower limb
II) Other causes :

Other causes can make there types of gait, and they are – Limping gait, Hysterical gait and Waddling gait
- Limping gait – Antalgic gait is a limp that occurs as a result of discomfort in the foot, knee, or hip. It is the most prevalent type of limp found in people. e.g., osteogenic, arthrogenic and congenital like Talipes equinovarus
- Hysterical gait – Conversion reaction causes a variety of strange gaits; the foot is commonly dragged or pushed ahead instead of raised while walking; the foot is frequently held dorsiflexed and inverted.
- Waddling gait – This is seen in congenital dislocation of hip joint.
IX. What are the signs of meningeal irritation :

- One of the signs of the pediatrician’s evaluated meningeal irritation related to 39 percent bacterial meningitis.
- There were no linked to a higher frequency of bacterial masings than neck rigidity and tripod phenomena in specific tests that triggered meningeal irritation, like Brudizinski’s and Kernige’s signs.
- Bacterial meningitis is associated with irritability and an overgrowth of fontanel more frequently in children of 1 year.
I. Neck rigidity :
At first, the patient’s head is supported by the hands and the palm is gently flexed until the patient’s chest touches the chin. When the neck is rigid, the neck cannot be flexed passively, and the examiner may feel spasm in the muscles of the neck.
In local causes such as cervical spine disease and increased intracranial pressure, neck rigidity is absent.
Meningitis triad – neck stiffness and headaches Photophobia
II. Neck stiffness :
- There are different causes of rigidity of the neck.
- Meningitis
- Meningism
- Rigidity of the brain
- Tetany
- Infiltration of Leukemic CNS
- Hemorrhage Subarachnoid
- Abcess of Retropharyngeal
- Posterior ICSOL(Intra cranial space occupying lesion)
- Trauma of the spine
III. Kering’s sign :
- With the left hand over a medial hamstring, the examiner flexes one of the legs on the hip and knee. Then the knee is stretched and the hip is bent.
- When spasm in the hamstring is resisted, the sign of Kernig is positive.
IV. Brudzinaski’s sign :
Brudzinski’s sign is one of the physically shown signs of meningitis. Hard neck rigidity causes the hips and knees of a patient to bending when the neck is flexed
V. Torticullis :
Torticollis is a problem that causes the head to tilt in with the neck muscles. Two Latin words are: tortus, meaning twisted and collum, meaning neck. It’s named “wryneck,” sometimes. If your baby is born, it’s known as a congenital torticolla.
Sternomastoid hematoma, cervical adenitis, medicine dystonia, brain tonsiller herniation are causes of torticulis.
X. How to examine Skull and spine :
Skull examination

During the skull examination we mainly focuses on eight things, and they are – Inspection (Size, shape, skin appearance, fontanels, Suture lines), Palpation, Percussion and Auscultation.
1. Inspection :
We check for size, shape, skull skin appearance, fontanels and suture lines.
- Size : This is determined by measuring the circumference of the head. Hydrocephalus is characterised by a large head, while Microcephaly is characterised by a small head.
- Shape : In various conditions, such as Craniosynostosis, Microcephaly, Hydrocephalus, Box-shaped head with enlargement (chronic subdural effusion), and Box-shaped head without enlargement, the normal shape changes (rickets)
- Skull skin appearance : Increased intracranial tension, venous sinus thrombosis, and venous sinus are all symptoms of this.
- Fontanels : Check the Anterior fontanel ; bulged anterior fontanels suggest enlarged ICT. Hypothyroidism, hydrocephalus, rickets, and osteogenesis imperfecta are all possible causes of an open anterior fontanel after the age of 18 months.If the Posterior fontanel stays open after 8 weeks of age, it merely indicates rickets, hydrocephalus, and hypothyroidism.
- Suture lines : Sutural gaps are evident in hydrocephalus, hypothyroidism, rickets, and microcephaly, as well as a visible suture line.
2. Palpation :
Rickets and prematurity cause a soft and ping pong ball sensation.
3. Percussion :
The Macewen sign, or cracked pot sound, is associated with increased ICT, TB, and meningitis.
Macewen Sign – Macewen’s sign, often known as the Macewen sign, is a symptom that can be used to diagnose hydrocephalus (excess cerebrospinal fluid) and brain abscesses. A cracked pot sound is produced by tapping (percussion) the skull near the junction of the frontal, temporal, and parietal bones. Sutures that have separated are indicated by a positive test. This is caused by increased intracranial pressure.
4. Auscultations :
For cranial bruit, auscultation is performed over the eyes, anterior fontanel, and temporal area.
- Soft bruit heard in – Meningitis, intracranial tumours, chronic haemolytic anaemia, subdural effusion, and normal youngsters up to the age of four years
- Loud bruit – This is abnormal, and it usually indicates a vascular abnormality.
Spine examination
Spine examination mainly holds three parts that is – Inspection, Palpation, percussion
- Inspection – We look for gibbus, tufts of hair, or any localised swelling over the spine, as well as kyphosis or scoliosis and dermal sinus.
- Palpation – Spina bifida should be palpated if it is present or suspected.
- Percussion – If you have any localised soreness, such as caries on your spine,
XI. How to check coordination :
The nervous system aids in the control and coordination of many bodily functions. The three types of nerves, cranial nerves, spinal nerves, and visceral nerves, run throughout the body and assist in the transmission and reception of electrical signals.
We value bodily coordination because it allows us to protect our bodies from hazardous stimuli such as hot objects. Voluntary activities are those that are committed by humans deliberately and require thought.
Tests to determine the coordination :
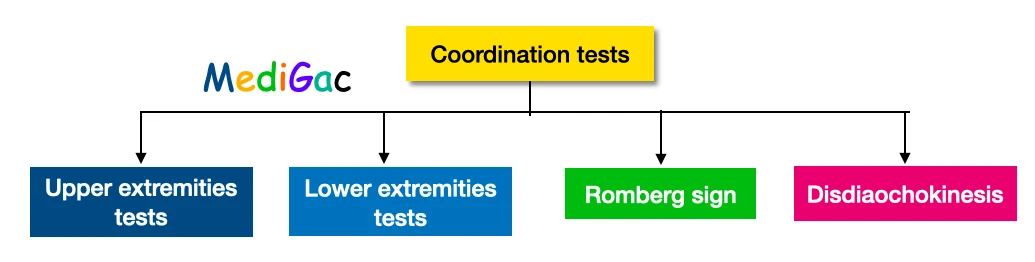
1. Tests for upper extremities :
We primarily focus on three upper limb tests: the finger-nose test, the finger-nose finger test, and Past pointing test.
- Finger-Nose test : The Finger-to-Nose-Test involves the examinee touching the tip of his or her nose with his or her index finger to assess smooth, coordinated upper-extremity movement. In one form of the test, the examiner extends his or her finger to the patient at roughly arm’s length.
- Finger-Nose Finger test : The examiner’s index finger is touched by the patient’s index finger. After that, the patient places their index finger on their own nose. The procedure is repeated numerous times, each time with the examiner shifting their target finger.
- Past pointing test : Both the subject and the examiners must sit face to face during this test. The patient is instructed to raise his hands in the air and touch the examiner’s index fingertips in front with his index fingers pointing up and down. The individual is then instructed to repeat the procedure, but this time with their eyes closed.
2. Tests for lower extremities :
- Knee-heel test : Test from heel to knee to shin Neurology A voluntary motor coordination test in which a person is instructed to slowly touch the knee of the opposite leg with the heel of the opposite leg. This test is affected by cerebellar impairment.
- Heel-toe test : The patient is instructed to walk in a straight line, one foot in front of the other (heel to toe), arms at their sides. If the patient falls, the examiner stays close enough to grab them. The examiner looks at the width of the base, the shift of the pelvis, and the knee flexion.
3. Romberg Sign :
The Romberg test assesses one’s sense of equilibrium. During a neurological exam, it’s often utilised to evaluate difficulties with balance, which is made up of the patient’s ocular, vestibular (inner ear), and proprioceptive (positional sense) systems.
- Positive romberg sign : The patient is able to stand with his eyes open, but he collapses with his eyes closed. From which a sensory deficiency can be detected
- Negative romberg sign : Even with his eyes open, the patient is unable to stand. And from this, we can detect a Cerebellar Defect.
4. Disdiaochokinesis :
The inability to perform quick alternate muscle movements is known as dysdiadochokinesia (diadochokinesia). Pronation/supination, fast finger tapping, opening and closing of fists, and foot tapping are examples of quick, synchronous movements.